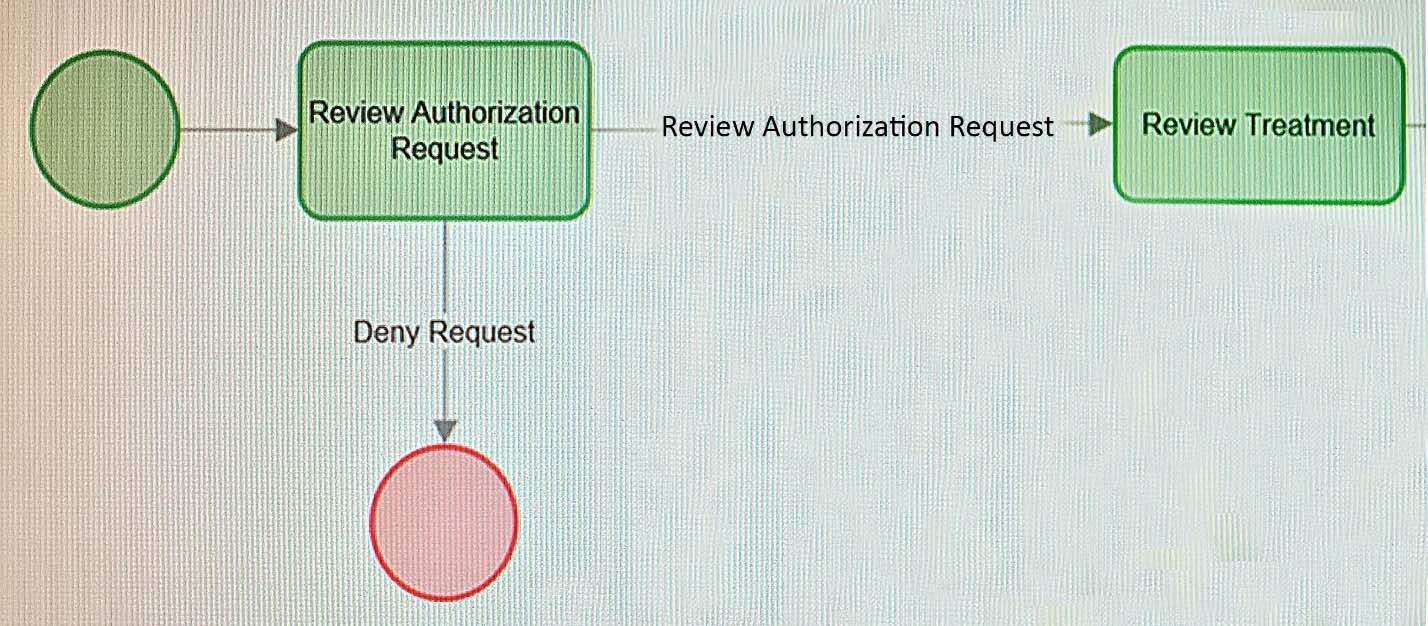
Before a member is admitted to a hospital, a health care organization reviews authorization requests for insurance coverage. An intake operator performs the
Review Authorization Request assignment to determine if the member qualifies for coverage.
If the member qualifies for coverage, the case advances to the Review Treatment assignment for review by a physician. When the case arrives in the physicians worklist, the system automatically sends the physician an email.
If the member is denied coverage, the system resolves the request. The system also automatically sends two types of correspondence to the member: a letter and an email notification.
How would you configure the process so that the system automatically sends an email to the physician when the case arrives at the physicians worklist?